NHS queues of nearly five million patients each month in England for a doctor’s appointment have put general practice back in the headlines. The Government has already stated its ‘expectation’ that all those who need a GP appointment can get one within two weeks.
Urgent appointments, meanwhile, should be on the same day, the Government said in its Autumn Statement of November 2022. However, breaking down what is or isn’t being achieved already and how to reduce NHS queues isn’t easy.
The Royal College of GPs says 85% of appointments happen within two weeks, with nearly half on the same day. It says the Government’s wait time target isn’t a fair measure if those appointments which take longer than two weeks are for routine matters.
Prof Kamila Hawthorne, who chairs the Royal College of GPs, says that GPs and their staff are working hard, and issues around delayed appointments are due to “decades of underfunding and poor resource planning.”
While the major parties and professional bodies seek to lay blame, patients may be more pragmatic and wonder if their practice is being run as efficiently as possible.
About 122 million GP appointments were booked in 2021/22, according to NHS England, and around 6.4% were missed – that’s around 7.8m appointments a year or 650,000 a month.
Earlier this year, the NHS asked hospitals to ensure they are sending appointment reminders, to improve processes for cancelling or rebooking appointments and considering remote appointments.
As Sir James Mackey, NHS National Director of Elective Recovery, says: “With NHS staff delivering more than two million outpatient appointments every week, and outpatients making up more than 80% of the overall waiting list, this drive to reduce missed appointments has the potential to make a huge difference in freeing up capacity and helping us deliver for patients.”
Technology can make a difference
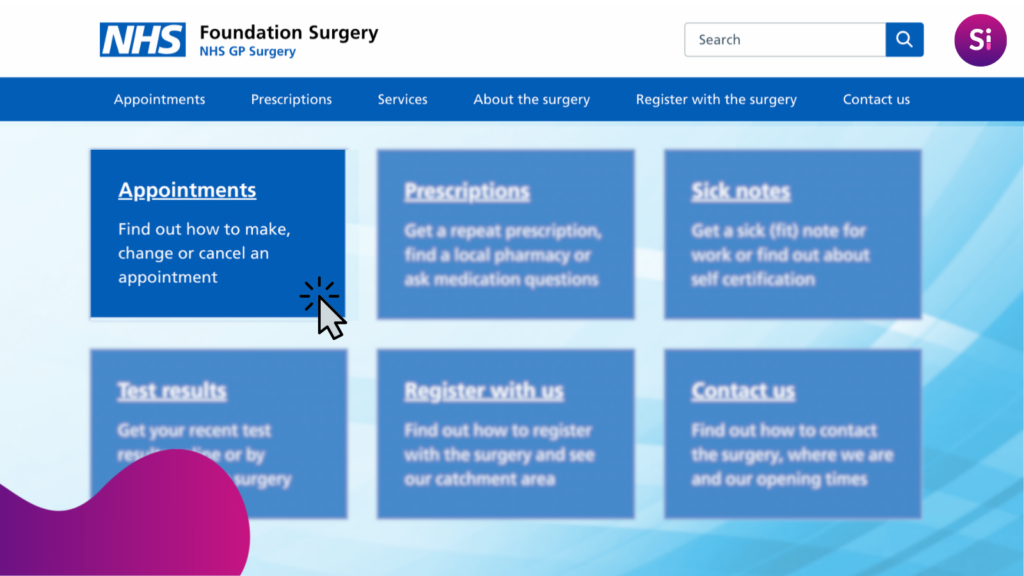
Many, if not all, of those initiatives can be used in primary care as well, with technology provided by Silicon Practice and others that can help GP surgeries step up to the challenge.
Silicon Practice sites have always prominently featured multiple ways patients can cancel appointments and contact their practice.
Not only can appointment reminders be sent by SMS, but text messages and emails can also be used to flag up availability so that patients who are prepared to be ‘on standby’ can be notified quickly when appointments become free.
NHS England has recently established benchmarks for ensuring patients find online healthcare provision, including appointment changes, easy to navigate and interact with.
Foundation sites are expected to achieve a 98% rating of the top NHS benchmark at launch and can be part of your strategy for reducing missed appointments.
Appointment scheduling efficiency will differ widely from geographical area to area, by PCN and, indeed, from surgery to surgery.
Increasing the use of video and phone consultations can reduce unnecessary visits to a surgery. Websites, such as those provided by Silicon Practice, can give patients control of recording blood pressure readings online and completing other healthcare assessments and reviews at times convenient to them.
Streamlining administrative tasks and reducing paperwork can bring benefits and will be one aspect of the approach that must be adopted across the UK if the situation is to improve.
Cash injections increasingly unlikely for NHS
Politics and how public funding is allocated is an inescapable part of the situation patients and NHS staff find themselves in.
In simplistic terms, increasing funding can help surgeries hire more staff, expand their facilities and invest in technology, which could lead to more efficient and timely care.
This can’t be untangled from the need to recruit and train more medical professionals, as well as training and supporting existing GPs, in many cases attempting to stem the flow of those into early retirement.
However, a massive boost in funding looks increasingly unlikely during the present cost of living crisis.
Offering GP services outside normal working hours, during evenings and weekends, has been seen as a way of distributing patient appointments more evenly and expanding the roles of nurses, nurse practitioners, and other healthcare professionals can free up appointments for GPs to see more complex cases.
Cooperation not conflict will help patients and clinicians
The NHS was created 75 years ago by a political party and, sadly, healthcare is always going to be a political football. Arguments on how much should be spent and on what are never going to cease.
In some cases, approaches will be tried and won’t work or, possibly more worrying, just be judged too costly to provide at the end of a trial period.
As website providers, we see this happening nationwide, and a one-size-fits-all approach is unlikely to work.
An evolving multifaceted approach is perhaps the key, as well as getting the message across to patients that they themselves have a part to play by keeping appointments and cancelling when unable to attend.
Learning lessons from successes and failures across Britain will be paramount if resources are to be used effectively.
Contact us to find out about Foundation.
Follow us on LinkedIn to ensure you don’t miss out on important news and updates.
post by Bruno Clements